Introduction
Once the diffusion of oxygen occurs across the alveoli, it is transported to the tissues for unloading through the bloodstream, while carbon dioxide diffusion through the alveoli out of the bloodstream follows for expulsion out of the body. Oxygen and carbon dioxide transportation occurs through different mechanisms.
Transport of Oxygen in the Blood.
Only a small portion (1.5%) of oxygen is transported through the bloodstream after diffusion. The remaining 98.5% of oxygen is bound to a protein known as hemoglobin and carried to the tissues.
Hemoglobin.
Hemoglobin (Hb), is a protein located in red blood cells (erythrocytes) made of four subunits, namely: two beta subunits and two alpha subunits.
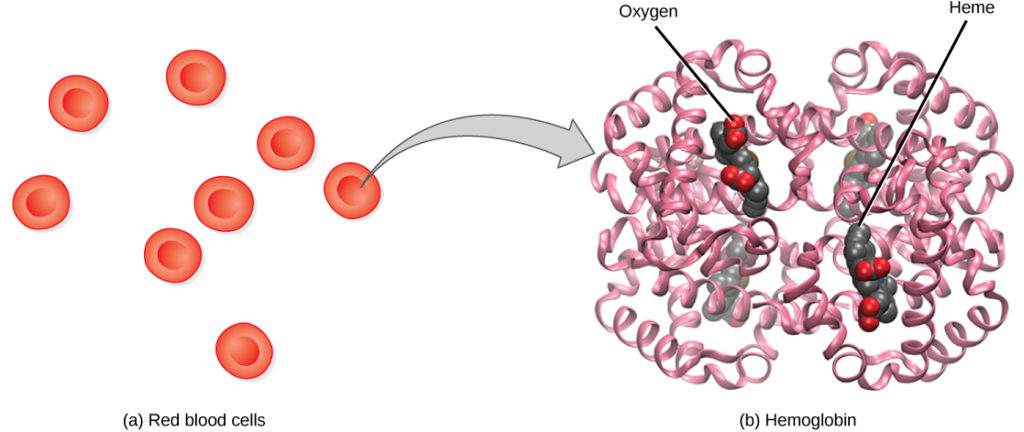
The heme group is surrounded by each of the four subunits and contains iron and binds a single oxygen molecule; therefore, each hemoglobin molecule binds four oxygen molecules. Molecules that have more oxygen bound to the heme groups appear brighter red, a condition that explains why oxygenated arterial blood where the hemoglobin carries four oxygen molecules looks brighter red compared to deoxygenated venous blood which appears darker red.
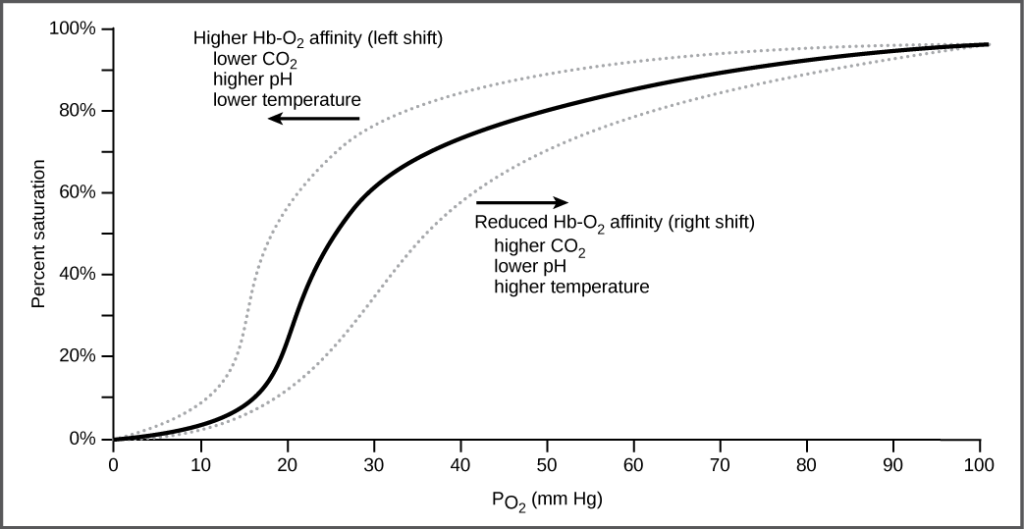
As oxygen binds to the hemoglobin, it changes its shape hence the binding of the second and third oxygen molecule is easier than the first one. The fourth oxygen molecule is then even more difficult to bind.
The oxygen dissociation curve is sigmoidal or S-shaped. This is because as the partial oxygen pressure increases, the hemoglobin is increasingly saturated with oxygen.
Transport of Carbon Dioxide in the Blood.
Transfer of carbon dioxide in the blood from the body tissues to the lungs can be achieved through three methods.
- Binding to the hemoglobin
- The direct dissolution into the blood.
- Transportation as a bicarbonate ion.
Properties affecting carbon dioxide transport.
- Carbon dioxide is more soluble in blood compared to oxygen, whereby 5-7% of carbon dioxide dissolves in the plasma.
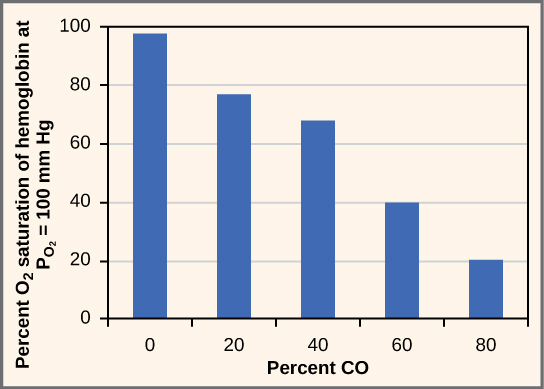
- Carbon dioxide binds to plasma proteins or enters red blood cells to bind on to hemoglobin, an activity which transports about 10% of carbon dioxide. Carbaminohemoglobin is the molecule that forms when CO2 binds to hemoglobin. When this molecule reaches the lungs, CO2freely dissociates from hemoglobin to be expelled from the body, an action that is possible since the binding of CO2to hemoglobin is reversible.
- The majority (85%) of CO2molecules are transported as part of the bicarbonate buffer system, where CO2diffuses into red blood cells. It is quickly converted into carbonic acid (H2CO3) by the carbonic acid within the red blood cells. Since carbonic acid (H2CO3) is unstable, it immediately dissociates into bicarbonate ions and hydrogen ions. Too much hydrogen ions alter the blood pH; however, hemoglobin binds to free hydrogen ions.
CO2+H2O⟷H2CO3(carbonic acid)⟷HCO3+H+(bicarbonate)
During expiration, hydrogen ions dissociate from hemoglobin to bind to the bicarbonate ion which the carbonic acid intermediate. This is followed by the conversion of the intermediate back into carbon dioxide by CA enzymatic action. The produced carbon dioxide is expelled through the lungs.