It has been made clear that the renin-angiotensin-aldosterone system “RAAS” plays an essential role in regulating the volume of blood and systemic vascular resistance, which together influence cardiac output and arterial pressure. As the name calls, there are three essential components to this system which are renin, angiotensin, and aldosterone. Renin is initially released by the kidneys, arouse the formation of angiotensin in the blood and tissues, and in turn arouses the release of aldosterone from the adrenal cortex. Renin is described as a proteolytic enzyme which is dropped into the circulation through the kidneys. Renin release is back up by sympathetic nerve activation, renal artery hypotension, decreased sodium delivery to the distal tubules of the kidney.
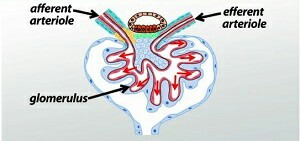
Juxtaglomerular cells joined with the afferent arteriole entering the renal glomerulus are the primary site of renin save and release. A decrease in afferent arteriole pressure results in the release of renin from the JG cells, whereas increased pressure displays renin release. Beta 1 -adrenoceptors found on the JG cells respond to sympathetic nerve stimulation by releasing renin. Specialized cells known as macula densa of distal tubules lie adjacent to the JG cells of the afferent arteriole. The macula densa senses the center of sodium and chloride ions in the tubular fluid. And When NaCl is push up in the tubular fluid, renin release takes place. In opposite, a reduction in tubular NaCl stimulates renin release by the JG cells. There is evidence that prostaglandins meaning PGE 2 and PGI 2 stimulate renin release in response to reduced NaCl transport across the macula densa. When afferent arteriole pressure decreased, glomerular filtration decreases, and this decrease NaCl in the distal tubule.
When renin is passed to the blood, it acts upon a circulating reduction, angiotensinogen, which undergoes proteolytic cleavage to produce the decapeptide angiotensin I. The vascular endothelium, in the lungs, carries an enzyme, angiotensin transform enzyme, which two amino acids are cleft off to produce the octapeptide, angiotensin II (AII), though some other tissues in the body can also produce AII.
AII has many important functions like constricts resistance vessels thereby increasing systemic vascular resistance and arterial pressure, stimulates sodium transport (reabsorption) at several renal tubular sites, thereby increasing sodium and water retention by the body, Acts on the adrenal cortex to release and aldosterone , which in turn acts on the kidneys to increase sodium and fluid retention.